Abstract
Introduction: Endotheliopathy is common pathologic findings in acute and long COVID-19, which is associated with the disease severity and predisposes to long-term complications. Previous studies have demonstrated that plasma levels of von Willebrand factor (VWF) and proteoglycan syndecan-1 are significantly elevated in patients with severe COVID-19. However, the role of these endothelial biomarkers for predicting a long-term outcome is still lacking.
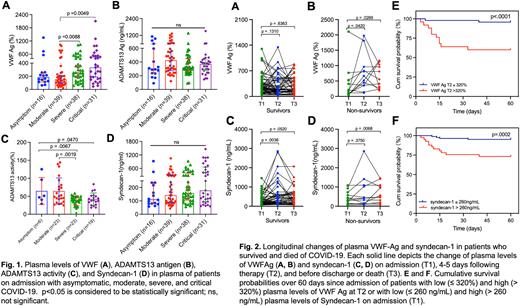
Patients and Methods:151 consecutive hospitalized patients between January and March 2022 at the University of Kansas Hospital with a confirmed SARS-CoV-2 infection by polymerase chain reaction were prospectively enrolled for the study. Whole blood anticoagulated with EDTA or sodium citrate was collected at least 3 times on admission (T1), 4-5 days following treatment (T2), and a few days prior to discharge or death (T3). Plasma levels of VWF antigen, ADAMTS13 antigen/activity, and syndecan-1 were determined using immunoassays or a functional assay. Kaplan-Meier survival analysis was performed to determine the predictive value of each biomarker for 60-day mortality.
Results. Of 151 patients with a positive PCR test for SARS-CoV2, 124 patients were studied and analyzed. These patients were categorized into an asymptomatic control, a moderate, a severe, and a critical group according to an updated World Health Organization (WHO) guidance. The admission plasma levels (median, IQR) of VWF in patients of critical (334%,164.7-526.2%) (p=0.0049) and severe (255%, 143.1-410.9%) (p=0.0088) groups were significantly higher than in those of moderate (153%, 186.3-240.1%) (Fig. 1A). Interestingly, no statistically significant difference in the admission plasma levels of ADAMTS13 antigen among all groups (p>0.05) (Fig. 1B) despite a significantly lower plasma ADAMTS13 activity (median, IQR) in patients with severe (39.8%, 30.0-49.3%) (p=0.0067) and critical (38.6%, 26.9-51.5%) (p=0.047) COVID-19 than in those with a asymptomatic disease (49.2%, 37.5-103.4%) (Fig. 1C). Furthermore, plasma levels of syndecan-1 on admission were not different among all groups (p>0.05) (Fig. 1D). Longitudinal analysis demonstrated that plasma levels of VWF antigen and syndecan-1 were persistently elevated from baseline in patients who died but not in those who survived (Fig. 2A-D). Kaplan-Meier survival analysis revealed that an elevated level of plasma VWF (> 320%) on T2 (p<0.0001) (Fig. 2E) or an elevated level of plasma syndecan-1 on admission (T1) (> 260 ng/mL) (p=0.0002) (Fig. 2F), but not 4-5 days following therapy (T2) or before being discharged home or death (T3) predicted the 60-day mortality rate.
Conclusions: Our results demonstrate significantly elevated plasma VWF antigen and reduced ADAMTS13 activity on admission in patients with severe and critical COVID-19. The dynamic change in plasma VWF or the initial plasma levels of syndecan-1 on admission predict the 60-day survival. The findings suggest that the additional therapeutic strategies may be needed to alleviate endothelial activation and damage to improve survival and long-term complications in patients with severe and critical COVID-19.
Disclosures
Zheng:Sanofi: Consultancy, Honoraria; Alexion: Consultancy, Honoraria; Takeda: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal